Saint John’s Health Center provides a multi-disciplinary approach to the treatment of cervical cancer. As experts in cancer diagnosis and translational research, our care teams can offer wide ranging services that are highly personalized to each patient, including access to clinical trials.
Our mission is to ease your way, providing the best and most comprehensive care for cervical cancer. We identify subtle characteristics of your disease to ensure the most accurate diagnosis, identifying the most optimal treatment for you. We believe, that by better understanding the genetic profile of the cancer, we can formulate highly effective treatment plans and thereby better outcomes. By also using minimally invasive techniques including laparoscopic and robotic surgery, highly precise radiation therapy delivery methods, and chemotherapy regimens that are designed to provide the best chance to control or halt cancer, we aim to minimize side effects so that you can maintain quality of life as much as possible. Our care teams are ready to support you.
How do you treat Cervical Cancer?
Depending on the location and stage of cervical cancer, its size, your age and overall health, one or more treatment methods may be needed to control the growth and spread of cancer. Common treatments include surgery, radiation therapy, chemotherapy, and targeted therapy. Our care teams will guide you through the entire process so that you are aware of all treatment options and clinical trials that are available to you. For cervical cancer symptoms and risk factors, please see Conditions: Cervical Cancer.
Surgery for Cervical Cancer
In early-stage cervical cancer, surgical options like a hysterectomy (removal of the uterus) or a trachelectomy (removal of the cervix), may be recommended to remove cancerous tissue and its ability to develop elsewhere in the body. Surgery is performed using minimally invasive, robotically assisted techniques in most cases. Surgery may require radical hysterectomy (removal of additional tissue along the sides of the uterus and cervix). Radical hysterectomy helps to reduce the likelihood of recurrence by addressing the tissue where cancer tends to spread at a microscopic level. A bilateral salpingo-oophorectomy (removal of both fallopian tubes and ovaries) will depend on your age and the extent of the disease. Fertility-sparing surgery can be performed under special circumstances where the cervix is removed but the uterus is preserved.
Radiation Therapy for Cervical Cancer
Radiation therapy is a common and effective treatment for various stages of cervical cancer, which is often used alone or in combination with chemotherapy (chemoradiation) in order to enhance its effectiveness. Radiation therapy (or radiotherapy) works by using high-energy rays or particles to damage the DNA of cancer cells, disrupting their ability to replicate, which caused cancer cells to die.
The side effects of radiation therapy can include fatigue, skin changes, nausea, diarrhea, and bladder irritation, which are typically managed with supportive care. Our healthcare team carefully plans and monitors the entire process of radiation treatment to maximize its benefits while minimizing potential side effects.
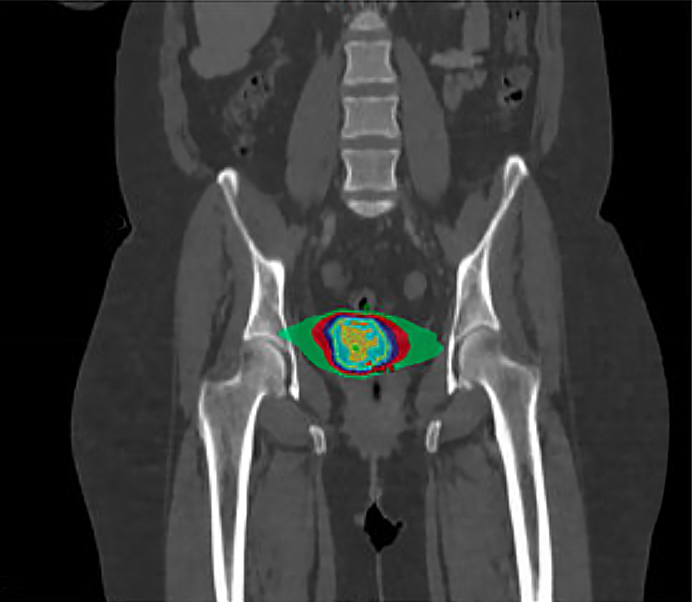
There are two main types of radiation therapy used for cervical cancer:
EBRT is the most common form of radiation therapy for cervical cancer. From outside the body, a machine directs an external beam precisely at the cancerous area, which may be given in daily treatments over several weeks. The goal of radiation therapy is to target the tumor while sparing as much of the healthy surrounding tissue as possible. Advanced techniques, such as image-guided and intensity-modulated radiation therapy (IG/IMRT), allow for more precise targeting and reduced side effects.
Brachytherapy:
Brachytherapy involves placing a radioactive source (or sources) directly inside or near the tumor. For cervical cancer, brachytherapy is often used in conjunction with EBRT. It allows for a high dose of radiation to be delivered directly to the cervix while minimizing exposure to surrounding tissue and structures. Brachytherapy can be delivered as low-dose rate (LDR) or high-dose rate (HDR) therapy, which gives the radiation oncologist more options in how to treat the cancer. HDR is more commonly used in cervical cancer due to its convenience and effectiveness, delivering a productive dose of radiations in fewer sessions.
Chemotherapy for Cervical Cancer
Chemotherapy for cervical cancer is used primarily to treat advanced stages of the disease, either as a standalone treatment or in combination other treatments. Chemotherapy involves using drugs to prevent cancer cells from replicating so that they die off, preventing spread to other parts of the body. The drugs used in chemotherapy work by targeting and destroying rapidly dividing cancer cells.
Neoadjuvant Chemotherapy: In some cases, chemotherapy is given before surgery to shrink the tumor and make it easier to remove. This approach is less common but may be considered in certain clinical situations where surgical complications are too great.
Adjuvant Chemotherapy: After surgery, chemotherapy may be used to kill any remaining cancer cells and reduce the risk of recurrence. This is typically considered if there are high-risk features found during surgery, such as lymph node spread or positive surgical margins (evidence of cancer cells directly adjacent to the primary tumor.
Palliative Chemotherapy: For metastatic cervical cancer or cancer that has recurred after initial treatment, chemotherapy is used to control symptoms and improve quality of life. In this setting, a combination of chemotherapy drugs, such as carboplatin and paclitaxel, may be used.
The specific chemotherapy regimen, including the choice of drugs and duration of treatment, depends on the individual patient’s condition and the goals of treatment. Side effects, such as nausea, fatigue, and increased risk of infection, are managed with supportive care and medication. Regular monitoring by the healthcare team also helps ensure the best possible outcomes.
Targeted Therapy for Cervical Cancer
Targeted therapy, which uses drugs to target specific cancer cell mechanisms, is an option for advanced cervical cancer. Targeted therapy takes advantage of imperfections in the cancer’s structure, genetic profile, or protein to allow other treatments, such as immunotherapy, to break through. The immune system thereby recognizes and attacks cancer cells more efficiently, which may also be explored as a treatment option. The choice of treatment is guided by a multidisciplinary team of healthcare professionals who discuss your case in tumor board meetings to devise how to tailor the approach to the individual needs and circumstances of each patient.
Common Questions for Cervical Cancer
How quickly does cervical cancer spread?
Cervical cancer spreads at varying rates, influenced by factors such as the cancer type and the individual’s overall health. Generally, cervical cancer progresses slowly over many years. Early-stage cancers, such as carcinoma in situ, may take years to develop into invasive cancer. However, once invasive, it can spread more rapidly to surrounding tissues and lymph nodes.
Timely diagnosis and appropriate treatment are crucial for effectively managing and treating cervical cancer.
What is the next step after being diagnosed with cervical cancer?
After being diagnosed with cervical cancer, the next step involves several key actions. First, consult with your oncologist to discuss the stage and specifics of your cancer. This will determine the treatment plan.
- Imaging and Tests: Your doctor may recommend further imaging and tests to understand the extent of the cancer.
- Treatment Planning: Based on your cancer’s stage, treatments could include surgery, radiation, chemotherapy, or a combination. A hysterectomy, which removes the uterus, is often suggested for early stages.
- Multidisciplinary Team: Engage with a multidisciplinary team including oncologists, radiologists, and surgeons to explore all treatment options.
- Support Systems: Seek support from family, friends, and support groups to help you through the treatment process.
How do you know if cervical cancer has metastasized to bone?
To determine if cervical cancer has metastasized to the bone, your doctor will recommend several diagnostic steps. First, report any persistent bone pain or fractures, as these can be signs of metastasis.
- Imaging Tests: Undergo imaging tests such as X-rays, CT scans, MRI, or PET scans. These help to visualize any spread of cancer from the cervix to the bones.
- Bone Scans: A bone scan can detect areas of increased bone activity, which might indicate cancer.
- Biopsy: In some cases, a biopsy of the suspected bone area may be necessary to confirm the presence of cancer cells.
- Blood Tests: Certain blood tests can detect markers indicating bone metastasis.
Early detection of metastasis is crucial for effective therapy planning. Treatments may include radiation therapy, chemotherapy, or drugs to strengthen bones and manage pain.
What happens if your cervix is removed?
If your cervix is removed as part of treating cervical cancer, it usually involves a hysterectomy, where the uterus is also removed. This surgery effectively treats early-stage cervical cancer and prevents its spread.
- Post-Surgery Recovery: You will spend several weeks recovering, focusing on rest and gradual return to daily activities. Pain management and drugs to prevent infection are part of the therapy plan.
- Health Impact: Removal of the cervix and uterus means you can no longer become pregnant. Menstrual periods will stop.
- Long-Term Effects: Regular follow-ups with your healthcare team are crucial to monitor your health and detect any recurrence.
- Hormonal Changes: If the ovaries are also removed, you may experience menopausal symptoms, requiring hormone replacement therapy.
- Emotional Support: Emotional and psychological support is vital. Seek help from support groups, counselors, or therapists.
At what stage is cervical cancer curable?
Cervical cancer is most curable when diagnosed at an early stage. In Stage I, cancer is confined to the cervix, and treatments are highly effective.
- Stage I Treatments: These may include surgery, such as a hysterectomy, to remove the uterus and cervix, or less invasive procedures like a cone biopsy. Radiation and chemotherapy can also be used.
- Stage II: At this stage, cancer has spread beyond the cervix but is still within the pelvic area. Treatments like surgery combined with radiation and chemotherapy offer a high chance of cure.
- Importance of Early Detection: Regular screenings, such as Pap smears and HPV tests, are crucial for early diagnosis. Early detection significantly improves the success rate of treatments and overall health outcomes.
- Preventive Measures: Vaccination against HPV can prevent most cervical cancers, further enhancing the chances of early and effective therapy.
Prompt and appropriate treatments at these stages can lead to a full recovery.
Does removing the cervix get rid of HPV?
Removing the cervix does not necessarily get rid of HPV (human papillomavirus). HPV is a viral infection that can remain in your body even after the cervix is removed through a hysterectomy. Here’s why:
- Virus Persistence: HPV can persist in other tissues of the genital area even after the cervix is removed. The virus can remain in vaginal or vulvar tissues.
- Immune System: Your immune system plays a crucial role in clearing the virus. In many cases, the body’s immune system can eventually eliminate HPV on its own over time.
- Monitoring: Regular follow-ups and screenings are still important after a hysterectomy if you had an HPV-related condition. Your healthcare provider might continue to monitor for any signs of HPV-related issues in other areas.
- HPV Vaccination: Vaccination against HPV can help prevent future infections and reduce the risk of HPV-related cancers.
While removing the cervix through a hysterectomy can treat cervical cancer or precancerous conditions, it does not eliminate the HPV virus from your body.
Call today to learn more about the diagnosis and treatment of cervical cancer. Our multi-disciplinary team is ready to support you.
If you have questions regarding cervical cancer or would like an expert second opinion, please call today or click here to schedule an appointment.