What is Colorectal Cancer?
Colorectal cancer (or colon cancer) usually develops slowly over several years, often beginning as a non-cancerous polyp on the inner lining of your colon or rectum. They can be referred to as colon cancer or rectal cancer depending on where they originate, though they have many aspects in common.
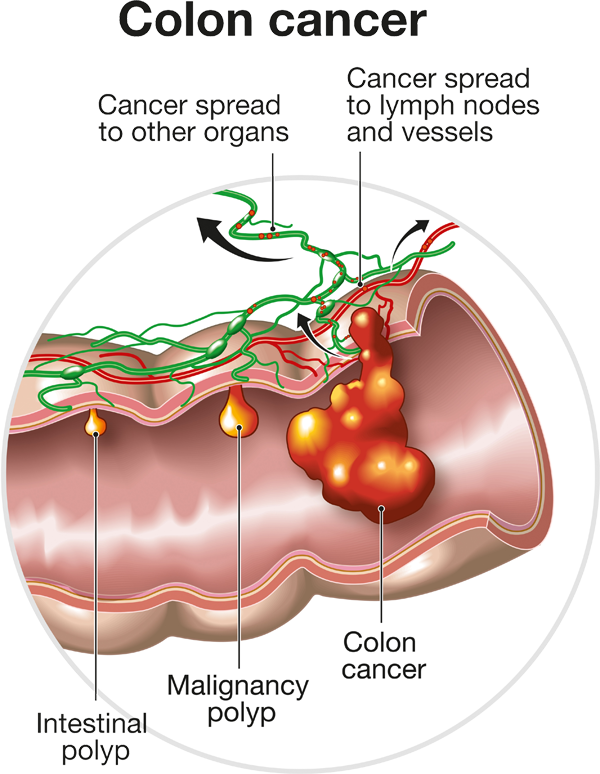
Most colorectal cancers arise in the sigmoid (the portion just above the rectum) or the right colon. They usually start in the innermost layer and can grow through some or all the several layers of tissue that make up the colon and rectum. The extent to which a cancer penetrates the various tissue layers determines the stage of the disease. A small percentage of colorectal cancers, usually hereditary forms of the disease, can cause large numbers of polyps to appear.
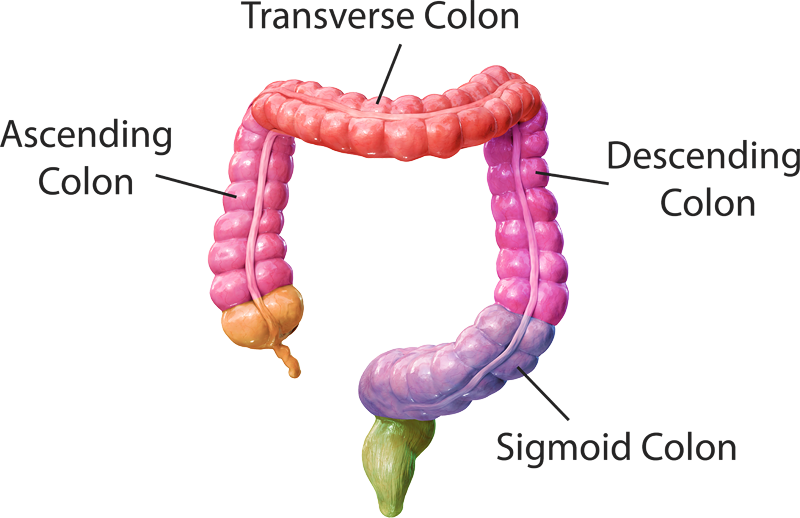
Colorectal cancers are usually contained within the colon, but when they become advanced the cancer can metastasize, or spread, to other organs. When colorectal cancer spreads, it tends to move to the peritoneum, liver, and lungs. The rectum is the lower six inches of the large intestine. The colon absorbs water and nutrients from food, and the rectum serves as the holding place for the stool. The colon is divided into four sections.
Sections of the Colon:
Each section of the color performs a specific function essential for digestion. Depending on the location of the cancer, the extent of treatment may vary. These sections include:
- Ascending colon – The start of the colon which absorbs the remaining water and other key nutrients from the indigestible materials
- Transverse colon – Follows the ascending colon and plays an essential role in digestion and the excretion of waste products
- Descending or left colon – Follows the transverse colon that stores feces that will eventually be emptied into the rectum
- Sigmoid Colon – The last part of the colon that connects to the rectum
What are polyps and are they cancerous?
Polyps are small growths that an take root on the inner lining of the colon or rectum. They can appear flattened or on a pedestal (stalk), known as a pedunculated polyp. Polyps are usually benign, or not cancerous. If not removed, they can evolve into cancer but don’t always. The development of cancer depends on the type of polyp. These include:
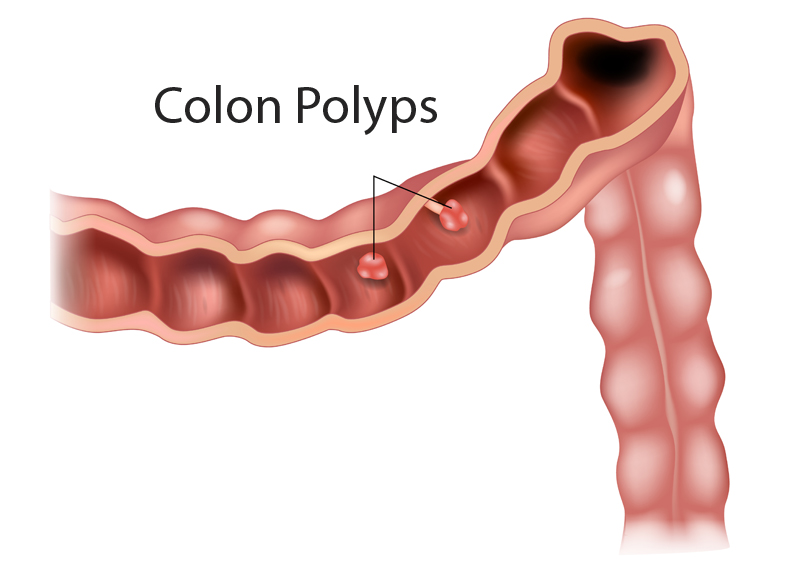
Adenomatous polyps
(adenomas) are polyps that can change into cancer and are referred to as pre-cancerous.
Hyperplastic polyps
and inflammatory polyps are usually not pre-cancerous.
Dysplasia
is another type of precancerous polyp that develops in the lining of the colon or rectum, where the cells look abnormal (but not like true cancer cells) when viewed under a microscope. These cells can change into cancer over time. Dysplasia can also be seen in people who have had diseases such as ulcerative colitis or Crohn’s disease for many years. Both ulcerative colitis and Crohn’s disease cause chronic inflammation of the colon.
At the Saint John’s Cancer Institute, we approach cancer treatment with a team of highly skilled physicians and nurses who focus on delivering the most effective and advanced care to help increase your chances of living a healthy life. We do that with innovative treatments that include minimally invasive laparoscopic and robotic surgical procedures, state-of-the-art radiation delivery systems, and the most novel medical therapies and clinical trials available.
Types of Colorectal Cancers and Tumors
More than 95 percent of colorectal cancers are adenocarcinomas — cancers of the cells that line the interior of the colon and rectum. Rarer types of tumors include carcinoid tumors, gastrointestinal tumors, and lymphomas.
The type of colorectal cancer you’re diagnosed with will help determine the optimal way to treat the cancer. Depending on whether you are diagnosed with colon cancer or rectal cancer, your treatment may be slightly different. Because rectal cancer surgery is more complex, due to the narrow confines of the pelvis, we take special care to avoid damaging sexual and bladder nerves as well as other structures. This is achieved through minimally invasive surgical techniques.
Adenocarcinoma:
Adenocarcinomas are the type of cancer cell found in 90 to 95 percent of colon cancer cases. Adenocarcinoma forms from the cells that help produce the mucus that lines the colon or rectum. They can invade the wall of the colon and then spread via lymphatic channels to surrounding lymph nodes. From there they can spread to the liver and the lungs.
Carcinoid Tumors and Neuroendocrine Tumors:
Carcinoid Tumors and Neuroendocrine Tumors typically occur in the small intestine and appendix and occasionally the rectum. They rarely occur in the colon.
Gastrointestinal Stromal Tumors:
Gastrointestinal Stromal Tumors can form anywhere in the digestive tract, though rarely in the colon.
- They can start in the special cells found in the wall of the GI tract, called the interstitial cells of Cajal (ICCs). ICCs are cells of the autonomic nervous system, the part of the nervous system that regulates body processes such as digesting food. ICCs are sometimes called the “pacemakers” of the GI tract because they signal the muscles in the digestive system to contract to move food and liquid through the GI tract. That’s why it’s important to have your gastrointestinal health.
- More than half of gastrointestinal stromal tumors start in the stomach. Most of the others start in the small intestine, but these types of tumors can start anywhere along the GI tract. A small number starts outside the GI tract in nearby areas such as the omentum (an apron-like layer of fatty tissue that hangs over the organs in the abdomen) or the peritoneum (the layer of tissue that lines the organs and walls of the abdomen).
- Not all gastrointestinal stromal tumors are cancerous. Some are benign (not cancerous) and don’t grow into other areas or spread to other parts of the body.
Lymphoma:
Lymphomas are cancers of immune system cells. They rarely begin in the colon or rectum.
Recurrent Colorectal Cancer:
Recurrent Colorectal Cancer is cancer that has come back after successful treatment, either in or near the colon or rectum, or in other organs.
Inherited Tumors
The two most common inherited colorectal cancer syndromes are hereditary nonpolyposis colorectal cancer (HNPCC) and familial adenomatous polyposis (FAP). They can affect both men and women, and in approximately 50% of children of people who carry this disease-causing gene.
Hereditary nonpolyposis colorectal cancer (HNPCC):
HNPCC is the most common form of hereditary colorectal cancer. If you’ve been diagnosed with HNPCC, chances are you have at least three family members and two generations with colorectal cancer.
- Not everyone who inherits the HNPCC gene will develop colorectal cancer, although the risk is very high — about 80 percent.
- People with HNPCC also have a higher risk of developing other cancers, such as kidney, ovarian, uterine, renal pelvis, small intestine, and stomach cancer.
- We can evaluate the pattern of colorectal cancer in your family to determine if the family has HNPCC. Families considered to be “HNPCC families” must display certain criteria indicating a pattern of colon cancer throughout generations.
Familial Adenomatous Polyposis (FAP):
FAP is a rare condition characterized by the presence of more than hundreds or even thousands of benign polyps or growths in the large intestine.
- It is thought to be present in about one percent of all people diagnosed with colorectal cancer each year. The polyps occur early in life, with 95 percent of people with FAP developing polyps by age 35, and are often detected in patients in their teens, with 50 percent developing polyps by age 15.
- If the colon is not surgically removed, there is a 100 percent chance that some of the polyps will develop into cancer, usually by age 40. While most cases of FAP are inherited, nearly a third of the cases are the result of a spontaneous or newly occurring gene mutation or abnormality. For those who develop a new gene mutation, it is possible to pass the FAP gene onto their children.
- In 1991, researchers made a significant breakthrough in the diagnosis of FAP. They identified the gene (APC) that is responsible for the condition. This gene mutation can be detected in 82 percent of patients with FAP. The exact lifetime risk of developing colon cancer in people who have inherited this gene abnormality is about 100 percent. Families in which this gene mutation occurs may or may not have one or more family members with colorectal cancer or polyps
Symptoms of Colorectal Cancer
Signs of colon cancer in women and men tend to be the same. If symptoms do occur, they may include the following:
- Rectal bleeding or blood in the stool.
- A change in bowel habits (such as diarrhea, constipation, or narrowing of the stool) that lasts for more than a few days.
- Abdominal pain.
- A continuous feeling of needed to have a bowel movement, which does not resolve after passing stool.
- Weakness
Some of these symptoms may be caused by other conditions, but you should see your doctor if they persist. Any incidence of rectal bleeding or blood in the stool should be brought to your doctor’s attention as soon as possible.
Colorectal Cancer Screening
Unfortunately, colorectal cancer often has no symptoms, making the importance of a colonoscopy even more significant for prevention.
Colorectal cancer can be a preventable disease thanks to screenings like colonoscopies, and, at-home stool tests. The screening age for colon cancer recently dropped from 50 years old to 45 years old.
Stool test:
A stool test examines the DNA in your stool for evidence of cells shed by colorectal cancer. The test is 92 percent accurate at detecting cancers in people with no symptoms.
Colonoscopy:
Colonoscopy is a type of clinical exam used to look for changes in the large intestine and rectum. During an exam, if a polyp is suspected of being cancerous, a biopsy can be done. The tissue obtained can determine if it is cancerous or precancerous.
Several factors can increase a person’s risk of developing colorectal cancer. The good news is that there are steps you can take to protect yourself.
What Are the Risk Factors of Colorectal Cancer?
Many factors can increase your risk of developing colorectal cancer. Some are beyond your control, but others can be affected by your lifestyle.
Age:
Colorectal cancer increases with age. The colorectal cancer screening age recently changed from 50 years old to 45 years old because the incidences are being found in younger populations, especially in certain ethnicities.

Polyps:
The presence of polyps in the colon increases risk, especially if they are large or if there are many of them.
Personal history:
If you’ve previously been diagnosed and treated for colorectal cancer, you’re at higher risk for developing it again.
Bowel disease:
Inflammatory bowel diseases (including ulcerative colitis or Crohn’s colitis) increase your risk of colorectal cancer because they inflame the colon over an extended period.
History of ovarian, uterine, or breast cancer:
Women who have had any of these cancers are at higher risk.
Ethnic background:
Black & African Americans, Jewish of Eastern descent, Native Americans, and Pacific Islanders are at a higher risk.
Family history:
Someone with a family history of the disease, especially a parent or sibling before the age of 55 or multiple relatives at any age, is at a higher risk.
Genetics:
About 20 percent of all colon cancer cases come because of specific genetic mutations. That’s why genetic testing is beneficial.
How Can I Reduce the Risk of Colorectal Cancer?
- Avoid a diet that is high in red, processed, or heavily cooked meats.
- Exercise weekly
- Maintain a healthy weight and avoid obesity, particularly having excess fat in the waist area, rather than the hips or thighs.
- Avoid cigarette smoking: Studies indicate that smokers are 30 to 40 percent more likely than nonsmokers to die of colorectal cancer because they are more likely to develop polyps.
- Avoid excessive alcohol consumption (8 drinks or more per week for women, 15 drinks or more per week for men).
Aspirin and other NSAIDs:
It is possible that aspirin or other non-steroidal anti-inflammatory drugs (NSAIDS) like ibuprofen, as well as some arthritis drugs, may lower the risk of colorectal cancer and polyps. Aspirin may even prevent the growth of polyps in people who were previously treated for early stages of colorectal cancer or who had previously had polyps removed from the colon. However, you should talk with us before starting any NSAID remedy.
Hormone-replacement therapy:
It is possible that hormone-replacement therapy (HRT) for women, which consists of estrogen and progesterone and is used after menopause, may also help reduce the risk of colorectal cancer. However, the decision to use HRT should be made between you and your doctor after discussing the potential benefits and risks.
Diagnosing Colorectal Cancer
The following tests may be used for colon cancer screening or to find out if the cancer has spread. Tests also may be used to find out if surrounding tissues or organs have been damaged by treatment.
Double-contrast barium enema (DCBE):
Barium is a chemical that allows the bowel lining to show up on an X-ray. A barium solution is given by enema, and then a series of X-rays are taken.
Blood test for carcinoembryonic antigen (CEA):
CEA is a protein, or tumor marker, made by some cancerous tumors. This test also can be used to find out if the tumor is growing or has come back after treatment.
Endoscopic Tests:
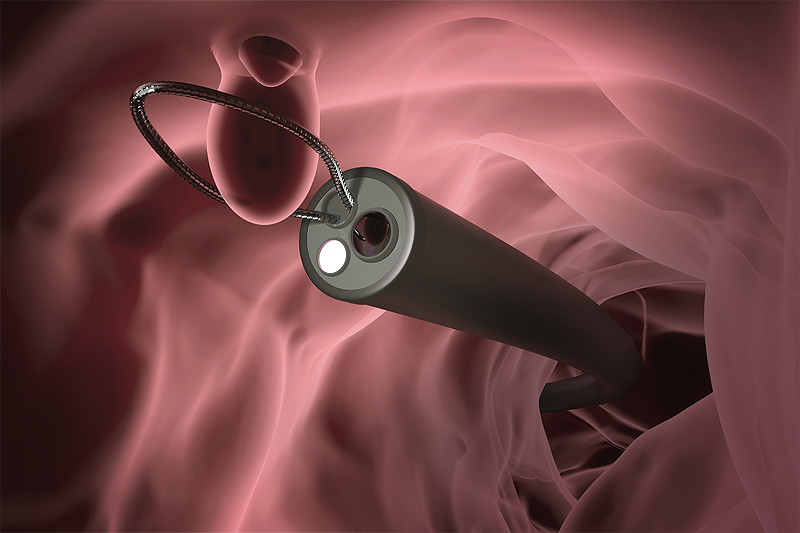
Sigmoidoscopy:
A tiny camera on flexible plastic tubing (sigmoidoscope) is inserted into the rectum. This gives the doctor a view of the rectum and lower colon. Tissue or polyps can be biopsied (removed) and looked at under a microscope.
Colonoscopy:
A longer version of a sigmoidoscope, a colonoscope can look at the entire colon.
Endoscopic ultrasound (EUS):
An endoscope is inserted into the rectum. A probe at the end bounces high-energy sound waves (ultrasound) off internal organs to take a picture (sonogram). Also called endosonography.
Fecal immunochemical test (FIT):
This take-home test finds blood proteins in the stool.
Fecal occult blood test (FOBT):
This take-home test finds blood in the stool.
Imaging Tests:
CT or CAT
(computed axial tomography) scan, is a noninvasive medical test that uses multiple x-rays to make a layered, 3D image of the area being examined.
MRI
(magnetic resonance imaging) scan, uses magnetic fields and computer-generated radio waves to create detailed images of the structures and tissues in the body.
PET/CT
(positron emission tomography) scan, is a test that involves radioactive tracers that are tagged with a specific molecule or protein. The imaging asses how the body’s organs are working on a cellular level. These tests are often combined with a CT scan, or MRI.
Virtual colonoscopy or CT
(computed tomography) colonoscopy, uses x-rays that looks for polyps, ulcers, and cancer from outside the body versus within. This is a less invasive approach to a colonoscopy, and does not require anesthesia, and takes less time.
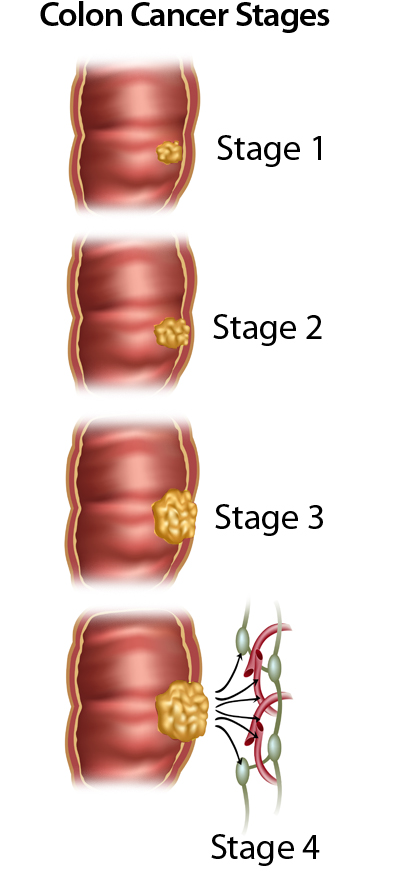
Colorectal Cancer Stages
If you are diagnosed with colon cancer, your doctor will determine the stage of the disease. Staging is a way of classifying cancer by how much disease is in the body and where it has spread at the time of diagnosis. This helps us to plan the best way to treat the cancer. Once the staging classification is determined, it stays the same even if the treatment works or the cancer spreads.
Stage 0:
Abnormal cells are found in the inner lining of the colon. These abnormal cells may become cancerous and spread into nearby normal tissue. Stage 0 also is called carcinoma in situ.
Stage 1:
Cancer has formed and spread into the first (submucosa) or second (muscle) layers of the rectal wall. It has not spread outside of the rectum.
Stage 2:
Cancer has spread outside of the rectal walls into the surrounding fat or nearby tissue. It has not gone into the lymph nodes. It is divided into stages: IIA, IIB, or IIC depending on the extent of local tumor involvement.
Stage 3:
Cancer has spread to nearby lymph nodes. It has not spread to other parts of the body. It is divided into stages IIIA, IIIB, or IIIC depending on the extent of local tumor involvement and the number of lymph nodes that contain cancer.
Stage 4:
Cancer has spread to other parts of the body, such as the liver, lungs, or ovaries. It is divided into stages IVA, IVB, and IVC depending on the number of different parts of the body to which the cancer has spread.
Colorectal Cancer Treatment Summary
Treatment for colorectal and rectal cancers requires a multidisciplinary approach: a surgical oncologist, a medical oncologist, a radiation oncologist, and a pathologist. Treatment for colorectal cancer can vary depending on whether the tumor is in the colon or rectum.
Minimally Invasive Robotic Surgery:
Minimally invasive robotic surgery for colorectal cancer requires smaller incisions and allows patients to return to normal activity within a short amount of time.
Chemotherapy:
Chemotherapy treatment for colorectal cancers is typically in more advanced stages and may require one or more treatment

Radiation:
Radiation therapy for colorectal cancers is typically in more advanced stages, which may require one or more treatments.
Immunotherapy:
Immunotherapy for colorectal cancers is typical in more advanced stages, which may require one or more treatments.
Targeted Therapy
Targeted Therapies for colorectal cancers are typical in more advanced stages, which may require one or more treatments.
Learn More
Click here for Colorectal Cancer Treatment.
Call today to learn more about Colorectal Cancer Diagnosis and Treatment. Our multi-disciplinary team is ready to support you.
If you have questions regarding Colorectal Cancers, please call today. Click here to request an appointment.