The Margie Petersen Breast Center at Saint John’s is committed to offering comprehensive evaluation and screening services. Our goal is to provide peace of mind and help you understand the changes you may be experiencing. We use a variety of imaging and diagnostic methods to fully evaluate any breast condition. These approaches include ultrasound, MRI, mammography, PET scans, and other tests.
Breast Ultrasound
For individuals under 30, ultrasound may be used to evaluate palpable findings before or in addition to a mammogram. Mammograms can be challenging to interpret in young women due to dense breast tissue, but tomosynthesis mammograms offer improved visualization. Most breast lumps in young women are benign, but imaging is essential to confirm this.
Ultrasound is also used to guide biopsies or cyst aspirations, providing real-time imaging to accurately locate and safely perform necessary tests.
If you have or anticipate scheduling a mammogram or breast ultrasound after a COVID vaccine, temporary enlargement of the underarm (axillary) lymph nodes can be expected. This is a normal reaction to some vaccinations; however, this can affect ultrasound results and / or biopsies. Click here to learn more, and about the questions we may ask.
Magnetic Resonance Imaging (MRI)
MRI is also the preferred method for detecting breast implant ruptures, especially silicone implants. It is recommended if you have been diagnosed with breast cancer to determine the extent of the disease, if a mass is felt but not detectable on other imaging, or if there is a suspected implant rupture. It is also used for individuals with a high risk of breast cancer, dense breast tissue, or a history of precancerous changes.
A Breast MRI May Be Recommended If:
- You’ve been diagnosed with breast cancer and the surgeons at Saint Johns want to determine the extent of the cancer or cancer in the opposite breast.
- You or your doctor can feel a mass or other lump in your breast, but it’s not detectable on mammogram or ultrasound.
- You have a suspected leak or rupture of a breast implant.
- You’re at high risk of breast cancer, defined as a lifetime risk of 20 to 25 percent or greater.
- You have a strong family history of breast cancer or ovarian cancer.
- You have very dense breast tissue and your prior breast cancer wasn’t detected on mammogram.
- You have a history of precancerous breast changes — such as atypical hyperplasia or lobular carcinoma in situ — a strong family history of breast cancer and dense breast tissue.
- You have breast cancer cells in your lymph node but your mammogram and ultrasound cannot find the cancer.
Breast MRI should be in addition to a mammogram or another breast-imaging test, and not as a replacement for a mammogram. Although it’s a very sensitive test, breast MRI can still miss some breast cancers that a mammogram will detect.
Mammography
Mammograms remain the most effective method for early breast cancer detection while being the only breast imaging technique proven to consistently reduce breast cancer mortality, allowing for timely treatment and improved outcomes. Consistency in mammogram facilities also aids radiologists in tracking changes in breast tissue, helping catch suspicious findings early and comparing prior images. Due to limitations with dense breast tissue, additional testing may be necessary for a complete evaluation.
If you have or anticipate scheduling a mammogram or breast ultrasound after a COVID vaccine, temporary enlargement of the underarm (axillary) lymph nodes can be expected. This is a normal reaction to some vaccinations; however, this can affect ultrasound results and / or biopsies. Click here to learn more, and about the questions we may ask.
Digital Mammography
Breast Density
California law requires physicians to inform patients if their mammograms show dense breast tissue, which can increase the risk of breast cancer. Breast density is visually determined by radiologists and classified into four levels by the American College of Radiology. Dense breasts have more breast and connective tissue compared to fat, which can make cancer detection more challenging. Additional imaging like ultrasound or MRI may be recommended for women with dense breasts.
Tomosynthesis “3D” Mammogram
Tomosynthesis, or 3D mammography, takes multiple low-dose images of the breast from different angles, providing a comprehensive view. This method is particularly effective for dense breasts and is more comfortable due to less compression. The Margie Petersen Breast Center uses digital tomosynthesis to detect cancer faster and more accurately.
Other Tests
These refined details can help provide a comprehensive overview of breast imaging and diagnostics, ensuring patients receive the most pertinent information for their care.
Positron Emission Tomography (PET) Scans:
PETS scans are not used for screening but can be useful for staging breast cancer, determining spread to nearby lymph nodes, metastasis (the spread of cancer to other parts of the body), and treatment response.
Computerized Tomography (CT) Scans:
CT scanning is not routinely used for breast evaluation but may ne utilized to verify if a tumor has spread to the chest wall, aiding surgical planning.
Thermography:
Thermography measures skin temperature to screen for cancer cells but is not a substitute for mammograms. Thermography also lacks scientific evidence for effective screening.
How to Read Your Imaging Report
The reports of your radiology exams usually contain three sections:
- Exam description and history –the type of exam, day it was performed, the reason it was performed and any important patient information
- Findings – a detailed description of the important findings on the exam including size, shape, location and changes
- Impression – a summary of the findings, what they mean and what to do about them Radiologists use standard terms in reports to describe the appearance of important findings.
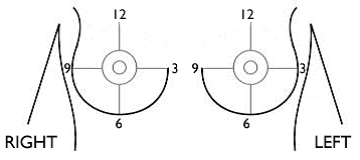
Some examples of those terms include mass, architectural distortion and calcifications. The radiologist will also describe the size, shape and location of important findings. The size and location can be critical to making decisions about the kind of operation and other treatments you might have.
The radiologist will also describe the size and location of a finding by indicating the distance from the nipple in centimeters. Centimeters are smaller than an inch. There are 2.54 centimeters in an inch.
The impression of the radiology report will often contain the abbreviation “Bl-RADS.” Bl-RADS stands for Breast Imaging-Reporting and Data System. Bl-RADS uses standard numbers to guide recommendations and convey our understanding of the important findings.
For example:
- Bl-RADS 0 means more imaging is needed before making a recommendation
- Bl-RADS 1 means the exam is normal
- Bl-RADS 2 means there is a finding that is benign
- BI-RADS 3 means a finding is probably benign and follow-up is recommended
- Bl-RADS 4 and 5 mean that there is a finding that is suspicious in some way and a biopsy is recommended
- Bl-RADS 6 means that we know for sure there is a finding that is cancer because a biopsy has already been done
A single lesion is likely to have different Bl-RADS numbers over time. When it is first seen, it usually is described as a 0. After more imaging it might be changed to a 3, 4, or 5. After the biopsy it may become a 6. Radiologists try to describe the location consistently so that everyone on the team knows that we are referring to the same lesion. The radiologist will use information from different examinations like ultrasound or MRI to help decide if a biopsy is needed or if there are additional findings that need to be evaluated. The different examinations allow us get different and important information about a finding so that we can help guide additional work up or treatment decisions.
Scheduling a Mammogram or Ultrasound after a COVID Vaccine
The COVID vaccine can temporarily enlarge underarm lymph nodes, potentially leading to unnecessary additional tests. To avoid this, breast imaging should be scheduled at least one day before the first vaccine dose or two weeks after the second dose. This guideline applies to patients without breast symptoms or concerns; those with concerns will be scheduled as normal.
Screening or Diagnostic Mammograms and Ultrasounds
In addition to the standard COVID screening questions we will also ask patients, “Have you had or will you be having a COVID vaccine?” If the answer is “yes” we will schedule your breast screening appointment at least 1 day BEFORE the FIRST vaccine dose or at least 2 weeks AFTER the SECOND vaccine dose.
We hope this approach will avoid unnecessary tests for our patient who have normal reactive lymph nodes. This only applies to patients who do not have breast symptoms and or concerns. For patient with a breast concern, we will schedule as normal, and our technologist will get your medical history.
Breast Cancer Screening Methods and Myths Webinar
Watch our breast cancer doctors at the Margie Petersen Breast Center at Providence Saint John’s, discuss the different types of breast cancer screening methods including, breast exams, mammography, ultrasounds, MRI, and biopsy, as well as share the facts for all the common breast cancer myths you’ve heard.