Did you know skin cancer is the most common type of cancer and melanoma is the most dangerous kind?
According to the American Cancer Society, about 96,480 new cases of melanoma will be diagnosed in the United States in 2019 with about 7,230 expected deaths. Melanoma is responsible for most of the skin cancer related deaths in the US. With the rates of melanoma on the rise over the past 30 years (increasing in numbers faster than other cancers) we want to help you identify the signs, symptoms and risk factors so you can detect it early in its course.
What is melanoma?
Melanoma is one of the most dangerous type of skin cancers. It is a tumor of the skin that is derived from cells that make pigment. The pigment released from melanocytes helps protect the skin from injury, typically that injury is from UV light (ie, sunlight). When the melanocytes in the skin are injured they tend to grow and express more of their pigment (usually manifest as tanning of the skin and darkening of the moles). When the injury to these melanocytes is so severe these cells lose their ability to stop growing and become cancer.
How do I know if I have melanoma?
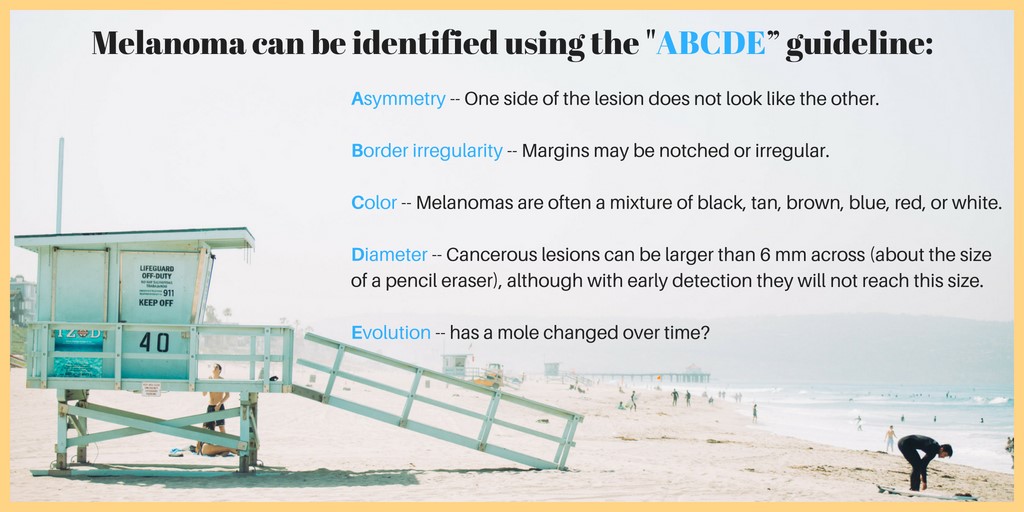
The appearance of skin cancer usually relates to the type. A basal cell carcinoma usually looks like a raised, smooth, pearly bump and is often found on the head, neck, or shoulders. While a squamous cell carcinoma is a well-defined, red, scaling, thickened bump on sun-exposed skin. Melanoma, on the other hand, can manifest as a new skin mole or as one that is changing in appearance. The mole can be flat or elevated off the skin surface. Usually, the moles are dark in color, dark brown or black but can be red or blue too. The best way for an individual to identify melanoma is to use the ABCDE’s guideline below and to see their primary physician or dermatologist for help:
What are the risk factors?
Skin cancer risk factors include: having a fair complexion with blonde or red hair, light skin, blue eyes and a tendency to sunburn or having a history of prolonged sun exposure. Other risk factors include excessive UV exposure, use of tanning beds and immunosuppression, or impairment of the immune system due to illness. There are several genes that are associated with the development of melanoma, suggesting that families can carry the risk of developing melanoma independent of sun exposure. Having had one melanoma puts an individual at increased risk of having another or more melanoma.
How is melanoma diagnosed?
Melanoma is diagnosed by a skin biopsy and not just the physical appearance of a mole. The skin biopsy specimen is examined by a pathologist, often a dermato-pathologist, an expert in examining skin tissue. The pathologist uses a variety of criteria to diagnosis melanoma. While a number of approaches have been used to help identify melanoma without performing a biopsy; there is no substitute for the skin biopsy.
What are the treatment options?
Skin cancer treatment is based on the type, size, location, and depth of the tumor, as well as the patient’s age and general health. Skin cancer and melanoma are usually treated with surgical removal and then pathology analyses of the skin removed to insure completeness. Some skin cancers can be treated with non-surgical approaches such as radiation or topical agents but melanoma is best treated with surgical removal. There are international accepted guidelines for excision of melanoma. If melanoma is recognized and treated early when it is confined to the skin, it is almost always curable. So early detection is key! However, if the melanoma is not found early in its development and has advanced or spread to other parts of the body, it becomes difficult to treat.
Melanoma can be life threatening if it spreads to lymph nodes or distant organs such as brain, lung and liver. Treatment options include surgery, radiation therapy, immunotherapy, targeted therapy or chemotherapy. In 2011 the first modern immunotherapy was approved in the United States. In 2014 a second class of immunotherapy drugs were approved by the US FDA for melanoma. These two classes of drugs called immune checkpoint inhibitors have revolutionized the treatment of metastatic melanoma and work by activating the immune system to the cancer. This property has allowed these immune checkpoint inhibitors to have a role in treating a variety of cancers aside from just melanoma. A second class of drugs can target growth stimulating pathways in melanoma cells. Several oral medications have been designed for targeting these growth stimulating pathways in melanoma cells. These drugs are highly selective for melanoma having particular gene alterations or mutations. These gene mutations are found only when the melanoma is tested specifically for these properties and are present in about of cases.
While we have made great steps forward in the last eight years treating melanoma with immune checkpoint inhibitors and targeted therapies we have not yet cured everyone. There are numerous clinical trials at the Saint John’s Cancer Institute using these and other newer therapies for melanoma.
You can learn more about the leading-edge treatment approaches for melanoma here: Learn More
How can I prevent melanoma?
Skin cancer prevention is all about protection! Select SPF 30+ products for both UVA and UVB light. If you are likely to sunburn, cover up with a long-sleeved shirt and wear a hat. Avoid excessive sun and UV exposure. Remember to avoid artificial tanning booths and conduct self-exams to check for your skin for changes. See your primary physician or dermatologist on a regular basis for a more detailed evaluation and skin biopsy if needed.
The Saint John’s Cancer Institute center for Melanoma and cutaneous oncology is one of the largest skin cancer centers in the US. We conduct research to help identify new and recurrent melanoma at its earliest stages and treat disease employing standard approaches or employing clinical trials in the more advanced cases or in ones where standard therapies have failed. Our team monitors the response to treatments and develops strategies for care.
We have published numerous groundbreaking melanoma studies including many that were created by the late Donald L. Morton, M.D., who established the institute’s melanoma program, and pioneered several surgical techniques. Dr. Morton was instrumental in the development of cancer vaccines that led to the modern immunotherapy approaches we use today.
As you enjoy the coming summer months, be sure to follow the melanoma prevention guidelines and help us continue to fight this dangerous cancer by supporting our scientific research and development of cutting-edge treatments.