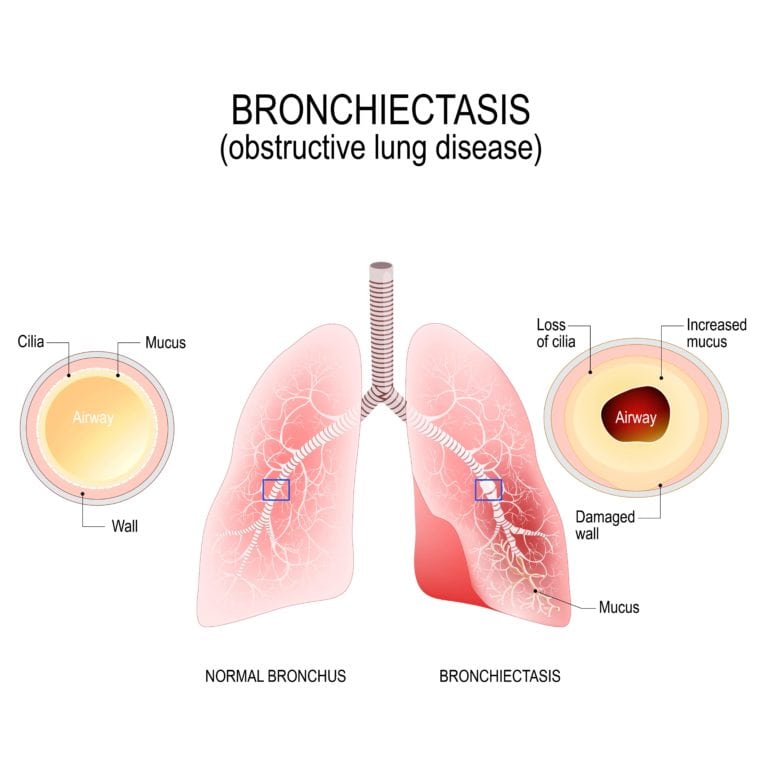
Bronchiectasis is the chronic inflammation of bronchi walls. It is characterized by thickening bronchi walls from inflammation and infection. When this condition flares up and causes breathing difficulties it is called exacerbations.
Bronchiectasis has two variations: cystic fibrosis (CF) bronchiectasis and non-CF bronchiectasis, and is usually part of a disease affecting the entire body. Some conditions that can cause bronchiectasis to develop are: humoral immunodeficiency (low levels of infection-fighting proteins in the blood), inflammatory bowel disease (Crohn’s disease and ulcerative colitis), Rheumatologic diseases (rheumatoid arthritis and Sjogren’s disease), Alpha 1-antitrypsin deficiency (genetic cause of COPD in some people), chronic obstructive pulmonary disease (COPD), HIV infection, and allergic bronchopulmonary aspergillosis (a type of allergic lung inflammation).
Treatment for bronchiectasis usually begins with antibiotics and macrolides, which are used to reduce inflammation in the bronchi. Mucus thinning medications and devices can also be used. However, when the patient is no longer responding to these various medications, surgical treatment will most likely be recommended. Since parts of the lungs that have been permanently damaged are unable to absorb antibiotics properly, surgery becomes a necessity to remove microorganisms that may be breeding in these damaged parts of the lung.
Surgical success is directly dependent on the removal of all diseased areas, early intervention to prevent resistant organisms from developing, pre- and post operative targeted antimicrobial therapy, and the anticipation of possible complications that may alter the planned surgical approach. Surgical treatment of bronchiectasis usually uses pulmonary resection, or the removal of part of the lung. Oftentimes, partial resection of the lung is completed with minimal morbidity and mortality. Most times, it can be surgically performed through the use of a video-assisted thoracoscope. However, in cases of diffuse bronchiectasis, especially in those with cystic fibrosis, a bilateral lung transplant is usually the only surgical option.
Ideal surgical candidates are those individuals who exhibit localized disease, have failed to control their condition with medications, and who have recurring symptoms that negatively affect their quality of life. In order to determine if you are an ideal candidate for surgery, Dr. McKenna will perform a pre-surgical assessment. This will begin with chest radiographs to detect the distribution of bronchiectatic alterations. Next, a bronchoscopy will be performed to identify the organism type affecting the lungs. In some cases, further measures may need to be taken depending on the type and severity of the organisms affecting the lungs.
During the surgery, the patient will be anesthetized using standard anesthetic technique with single-lung ventilation. An arterial line and urinary catheter will also be placed. Most surgeries begin with a bronchoscopy to clear the airway and optimize ventilation. Then, depending on the nature of the procedure being performed, pulmonary resection will begin either through an thoracotomy (open) approach or via a video-assisted thoracoscopic approach. While the video-assisted thoracoscopic approach is more minimally invasive, it may not always be the best option for every particular case.
If you have been diagnosed with bronchiectasis or believe that you may be experiencing symptoms of bronchiectasis and would like more information, schedule a consultation with Dr. McKenna today. In the case of bronchiectasis, the sooner you being treatment, the better the outcome.