Welcome to Vasek Polak Radiation Oncology
At the Vasek Polak Radiation Oncology Department at Providence, Saint John’s Health Center, we provide comprehensive, state-of-the-art radiotherapy services. In our community hospital setting, our care teams offer an extensive level of care and ongoing support. Radiation therapy is used to treat about every type of cancer, including some noncancerous (benign) tumors. We treat each patient as family with compassion throughout their treatment and recovery while working with other specialists to provide a multi-disciplinary approach.
How does radiation therapy work?
Radiation uses high-powered X-rays and other radioisotopes to destroy cancer cells by disrupting their ability to reproduce. The goal is to isolate the treatment area while minimizing radiation to the normal surrounding tissues. External beam radiation involves the use of imaging and other motion-tracking technologies to ensure the accurate delivery of radiation for each treatment.
When is radiation therapy prescribed?
Radiation is prescribed when the radiation oncologist believes there will be a medical/health benefit aside from other treatments. Though radiation can be used as a standalone treatment, it is often part of a collaborative or phased approach that involves other specialists, such as surgeons and medical oncologists. For example, radiation may be involved in shrinking the size of a tumor, making it less complicated to remove using surgery. After the surgery, the medical oncologist may indicate the need for chemotherapy to ensure that any remaining cancer cells are destroyed. Once involved, the radiation oncologist will develop a treatment plan that is specific to each patient before starting treatment.
Radiation Oncology and Support Team
There are several key individuals at our center who work together to provide the most comfortable treatment experience possible. Each provides a critical role in the development and delivery of radiation therapy.

Radiation Oncologist
The radiation oncologist is a board-certified physician who specializes in the treatment of cancer by using radiation therapy. They develop patient treatment plans and work with other staff, such as the radiation physicist, dosimetrist, therapists, and nurse, to ensure quality care. Each treatment plan is patient-specific and can vary in the number of treatments depending on the cancer type, location, and stage.
Radiation Oncology Nurse
The radiation oncology nurse specializes in cancer care and helps coordinate your treatment with physicians and other staff. As an Advanced Oncology Certified Nurse Practitioner, certified by the Oncology Nursing Certification Corporation, they are at the center of oncologic care management. They provide patient education and can refer patients to other healthcare specialists as needed. The nurse is there to guide patients through the entire radiation therapy process.

Radiation Physicist
The radiation physicist holds a Ph.D. or master’s degree in medical physics and may be certified by the American Board of Radiology or the American Board of Medical Physics. The physicist is responsible for the measurements and doses involved in radiation therapy and other related calculations, ensuring a high degree of safety for all patients treated at our center. They work closely with the radiation oncologist and dosimetrist to ensure the highest degree of safety for all patients.
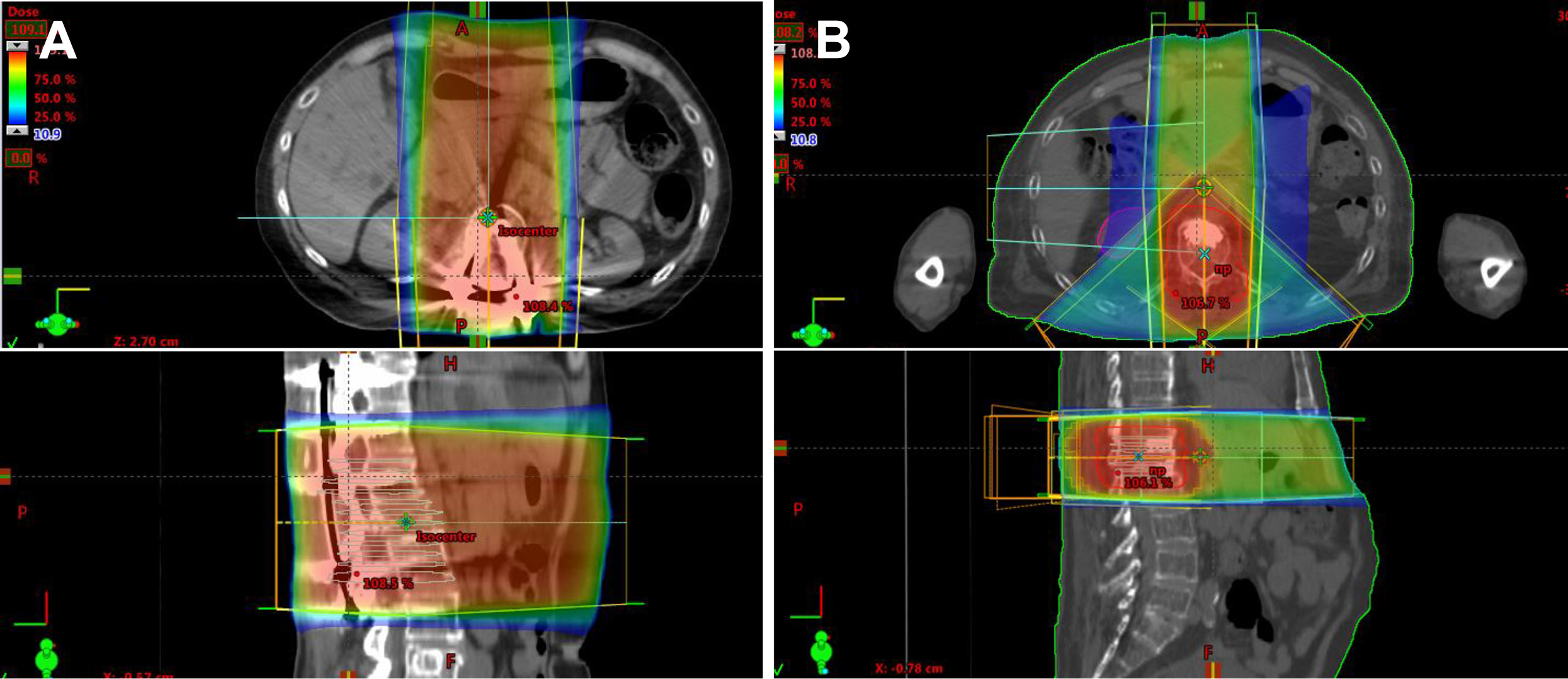
Dosimetrist
The dosimetrist is certified by the Medical Dosimetrists Certification Board and appreciates the radiation treatment process and equipment. They work closely with the medical physicist and radiation oncologist and ensure the accurate delivery of the prescribed dose of radiation while documenting pertinent information and verifying the mathematical accuracy of all calculations. They essentially map out the radiation delivery path using CT scans and MRIs to create a customized treatment plan for each patient. Using specialized computer software, they calculate the exact amount of radiation needed for each patient based on their tumor location and size, considering factors like beam angles and treatment fractionation.
Radiation Therapists
The Radiation Therapist is trained and certified in radiation therapy by the American Registry of Radiological Technologists (ARRT). Under the direction of the radiation oncologist, the therapists are responsible for delivering the prescribed treatment. They interact with the patient daily and ensure that the treatment experience is pleasant and worry-free. During treatment, the therapist helps the physician use CT scans and other imaging methods to localize the treatment area.
Nutritionist
Depending on the type of treatment you may receive, a nutritionist may be recommended. For example, if your treatment involves your head and neck area or the gastrointestinal tract, a nutritionist can provide guidance that can help maximize your recovery, factoring weight management, hydration, oral supplements, changes in taste, and treatment-related side effects.

Social Worker
Oncology social workers are licensed professionals who counsel people affected by cancer, providing emotional support and access to practical services. The social worker helps connect patients and their family members to all other components related to oncologic care and patient well-being, including individual counseling, navigating care resources and support groups, locating services that can help with in-home care or transportation, as well as guiding patients through the disability process or other forms of support, such as financial assistance.
What is the Radiation Treatment Process?
Before treatment starts, a clinical consultation and evaluation will be scheduled with the radiation oncologist, who will provide information and answer any questions you may have. The physician will review your medical records, body scans, and other test results and will perform a physical examination. If radiation is recommended, you and your referring physician will receive additional information, and a treatment plan will be developed.
Once the plan is complete, a simulation is needed to obtain body and tissue density measurements to further optimize the treatment before radiation delivery starts. Once the simulation is complete, radiation delivery is provided by the radiation therapists, who follow the plan and use CT scans obtained during the simulation to provide accurate treatment. For a more complete account of the radiation treatment process, please see Radiation Treatment Process below.
Radiation Treatment Process
Learn more about the radiation treatment process, the roles and responsibilities of the care team, and the various technologies associated with radiotherapy.
Common External Beam Technologies
Radiation treatment is a multi-step process involving several technologies to ensure accurate and safe treatment. Some treatments may require a single dose of radiation, such as Intra-operative Radiation Therapy, IORT, an outpatient procedure for breast cancer, while others may take up to 9 weeks (about two months). The amount of treatment and the dose of each treatment are determined by the radiation oncologist and verified by the dosimetrist.
IMRT
Intensity-modulated Radiation Therapy, IMRT, allows the radiation dose to be shaped to the contours of the tumor, minimizing exposure to healthy tissue. This is achieved with the Multi-leaf Collimator, MLC, which is a computer-controlled device inside the head of the linear accelerator made up of many closely spaced, movable leaves that adjust independently to block parts of the beam. When active, the collimator moves organically, creating polygons that match the tumor’s profile even as the machine rotates.
IGRT
Image Guided Radiation Therapy, IGRT, the standard of radiation treatment, involves taking high-quality images before each radiation therapy treatment session to increase the accuracy and precision of the radiation delivery. This ensures that any changes in the body or the tumor are accounted for.
Cone Beam CT
The Varian Edge is also equipped with Cone Beam CT, CBCT, and fluoroscopy, advanced on-board imaging systems that provide high-resolution images that guide treatment planning and delivery. Such imaging allows for the visualization of tumors and surrounding structures immediately before and during the treatment, further ensuring targeting accuracy.
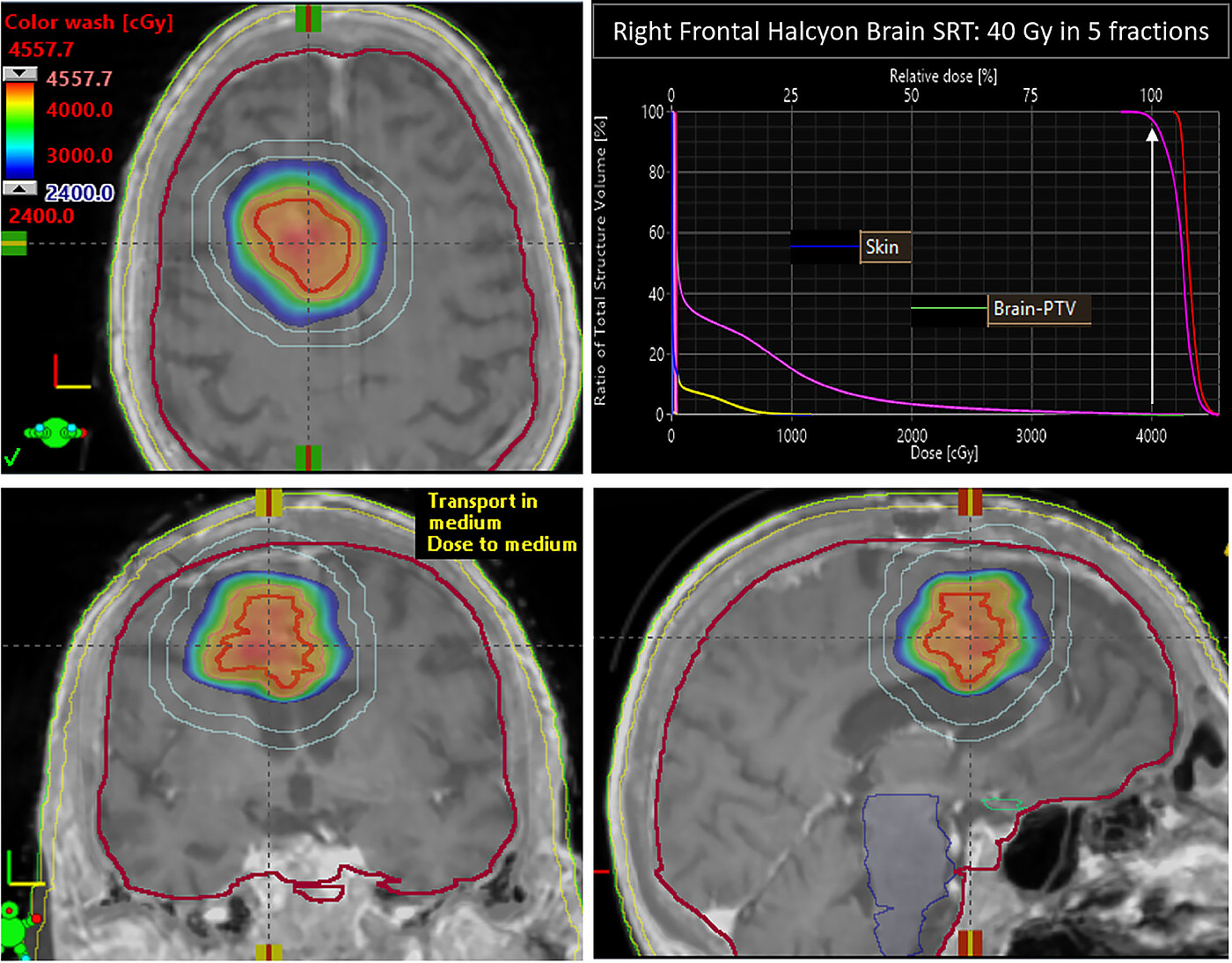
Stereotactic Radiosurgery
Stereotactic Radiosurgery (SRS) delivers a high dose of radiation to small, well-defined tumors in a single dose or in just a few sessions such as with treating pituitary or spine tumors or brain metastasis. The term radiosurgery is derived from this treatment method which has such a dramatic reducing effect on the tumor, that the changes are considered “surgical.” SRS may be used as the primary treatment when a tumor is inaccessible by surgical means or as a boost or adjunct to other treatments for a recurring or malignant tumor.
Stereotactic Body Radiation Therapy
Stereotactic Body Radiotherapy (SBRT) refers to a technique that treats tumors in the body, such as small tumors in the lung, liver, pancreas, and other areas of the body outside of the brain. With the capability of higher doses of radiation, treatment is completed over a few sessions compared to several weeks or more as compared to conventional therapy.
Volumetric Arc Therapy
Volumetric Modulated Arc Therapy, V-MAT, involves radiation delivery in a continuous 360-degree rotation around the patient, providing highly conformal dose distributions. This technique reduces treatment delivery time (in as little as 10 minutes), which improves targeting accuracy and patient comfort.
Internally Delivered Radiotherapy
Internal radiation, or brachytherapy, involves treatment near or inside the affected tissue. There are two types of brachytherapy: intracavitary treatment and interstitial treatment. With intracavitary treatment, the radioactive sources are put into a space near the tumor, such as the cervix, vagina, or esophagus. Such is the case with ovoid radiation treatment, also known as tandem and ovoid brachytherapy. Radioactive material may be placed within a tube inside the body and removed when the prescribed dose has been reached.

Low Dose Rate Brachytherapy
Low Dose Rate (LDR) brachytherapy is a type of internal radiation therapy where small radioactive seeds or sources are placed inside or near the tumor. These seeds emit radiation at a low dose rate over an extended period, typically several months. The goal is to deliver an ideal dose of radiation directly to the cancer cells while minimizing exposure to surrounding healthy tissues. LDR brachytherapy is commonly used to treat prostate, cervical, endometrial, and skin cancer, as well as brain tumors.
High Dose Rate Brachytherapy
High Dose Rate Brachytherapy (HDR) is a powerful form of internally delivered radiation therapy that destroys many types of cancers, including skin, prostate, and breast.
With any radiotherapy technique, the goal is to conform the dose to the size and shape of the target while limiting side effects by sparing the surrounding healthy anatomy. In brachytherapy, radiation is limited to the target area.
Other forms of Radiotherapy Delivery
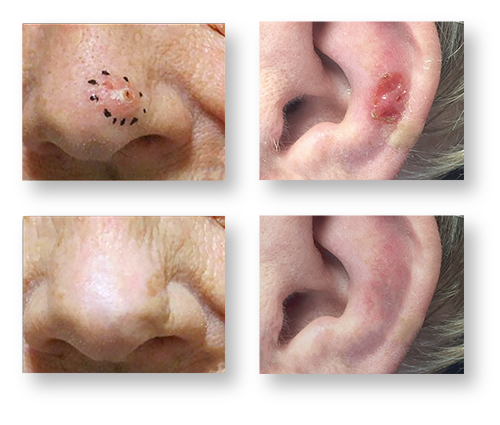
Superficial Radiation Therapy
Superficial Radiation Therapy, SRT, is another low-energy, outpatient radiation treatment used to treat cancer and other conditions on or near the skin’s surface. SRT can be used to treat basal cell carcinoma and squamous cell carcinoma and can be used on almost any part of the body.
Leading the way in radiotherapy for skin cancers and dermatological conditions, Providence Saint John’s Health Center has the only superficial treatment unit on the West side with the ability to treat skin lesions non-surgically, with minimal side effects and excellent cosmesis. Superficial Radiation Therapy (SRT) is a proven surgical method for non-melanoma skin cancers.
Clinical conditions treated include:
- Basal cell carcinoma
- Squamous cell carcinoma
- Keloid’s (following surgical excision)
- Mycosis fungoides
At Vasek Polak Radiation Oncology Department at Saint John’s Health Center, we are ready to support you throughout your entire journey, understanding that it requires a highly experienced team to effectively care for patients affected by cancer. Please contact us if you have questions.
If you have questions regarding radiation treatment or would like an expert second opinion, please call our center.